What Are Bedsores?
They owe their origin to the observation that patients who were bedridden and not properly repositioned, would often develop ulcerations on their skin, usually over bony prominences. Such sores, which result from prolonged pressure, are also called
“decubitus ulcers” or “pressure ulcers/sores”.
Bedsores can develop within short periods – hours – and progress rapidly and are difficult to heal, till the inciting factor is removed.
So bedridden patients, paralyzed patients who cannot move by themselves or those who are unconscious and unable to feel the pain of sustained pressure are especially at risk.
Common Sites for Bedsores
Importantly bed sores do not always result from being in bed as the name implies. The location of the ‘bed sores’ usually depends upon the position of the patient.
Sacrum & Lower Back
Tailbone area under prolonged pressure on mattress.
Heels & Hip
Heels and hip pressed cause circulation blockage.
Pressure ulcers may also develop in a number of other areas, including the spine, ankles, knees, shoulders, and head, depending upon the position of the patient. Prolonged sitting may also contribute to formation of such ulcers especially in wheelchairs.
Causes of Bedsore
Sideways movement between two surfaces is shear. Your skin moves in one direction and the underlying bony and tendinous tissue moves in the opposite direction of movement. This happens when you slide down in a bed or chair. This force tears the capillaries and superficial skin layers and predisposes to the development of such wounds.
Risk Factors
Pressure sores/BEDSORES are more likely to develop persons who are at higher risk due to one or more risk factors. The common ones being:
Complications
Pressure sores can trigger other ailments, cause patients considerable suffering, and be expensive to treat.
Complications Listed Below:
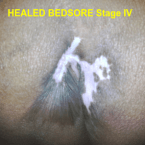
Treatment
The best treatment outcomes will result from using a multidisciplinary team of specialists, to ensure all problems are addressed. Units specializing in wound care like Savelegs Diabetic Foot & Wound Care Centre, are able to give better results when compared to other units.
Opening Hours
|
Monday |
1 PM – 3 PM |
|
Tuesday |
CLOSED |
|
Wednesday |
1 PM – 3 PM |
|
Thursday |
CLOSED |
|
Friday |
1 PM – 3 PM |
Closed on Tuesday, Thursday, Saturday & Sunday
